In Many Minneapolis Schools, the Therapist is Just Right Down the Hall
When Cathy Moen’s son, Elijah, was in first grade, he was diagnosed with attention deficit hyperactivity disorder. She took him to the pediatrician, who put him on medication and suggested therapy.
The medication part was easy. But getting him therapy proved more difficult — not because Moen couldn’t find a therapist or didn’t have insurance, but because of logistics.
The appointments were always during the day, and between her work schedule and the traffic, it was nearly impossible for them to make it.
But she soon learned Elijah was able to see a therapist in his Bloomington school. More than 15 years ago, Minneapolis Public Schools helped pioneer a national model of bringing community mental health care directly to its students. Today, most of the public schools in Minneapolis — more than 50 of them — have a therapist on site, and many other districts, like Elijah’s, have followed suit.
These days, Elijah’s therapist simply walks down the hall and pulls him from class.
“This is like a godsend,” said Moen.
The family’s health insurance pays for the care the same way it would if the student were being seen in the clinic. The school program was designed so that no student in need will be turned away for lack of insurance.
The Minneapolis program has also provided a road map for schools across the country as more administrators realize that mental health is as important to students’ future success as academics. Studies have shown that students are more likely to show up for appointments when the therapists are on-site.
More and more states are making mental health care in schools a priority. At least two states have recently passed laws that require schools to teach mental health. And more are considering it.
But the benefit of having a therapist on-site goes beyond just getting students to see a therapist. In Minneapolis, it’s also helped make mental health a school-wide priority — and helped get counselors, teachers and others more involved, said Mark Sander, who helped start the district program.

Mark Sander is the director of school mental health at Hennepin County and Minneapolis Public Schools.
Christine T. Nguyen | MPR News
“Those teachers start learning more and more [about mental health],” said Sander, who directs school mental health for the district and the county.
He said as they learn more about mental health, teachers are feeling like, “‘OK, I get it. And now, you know, I’ve got this other student who’s not diagnosed with anxiety but has some of those anxiety features. And now I know how to better support them.”
At South High School in Minneapolis, the therapists sit in the school clinic, the same one where students go if they feel sick during the day or to get a physical so they can play sports.
The issues the students bring to the therapist run the gamut from stress about grades and colleges to anxiety related to a bad situation at home.
Farah Hussein is a therapist at South. She said it’s hard being a teenager, and she tries to help.
“There’s a lot of conversations about, ‘Who am I? Where do I fit in the world? Where do I belong?’ and just a lot of distress in exploring that,” she said.
All of this has important implications for the students’ well-being beyond just their mental health.
Sharon Hoover, who co-directs the National Center for School Mental Health at the University of Maryland School of Medicine, said more schools are collecting data on outcomes of in-school mental health programs, and the results are clear.
“They are more likely to have good attendance and to graduate and to get improved grades. We even have documentation of having better standardized test scores when you put universal systems in place like classroom-wide social emotional learning,” she said, all of which makes for happier, better adjusted students.
Cathy Moen, the mother whose son, Elijah, is in therapy in school, said she doesn’t know if it’s the medicine, or the therapy, or just that he’s growing up, but she — and his teachers — are already seeing a difference.
In International Falls, the last psychiatrist for 100 miles just retired
When Dr. Jeff Hardwig started his job as a psychiatrist in his hometown near the Canadian border, he wasn’t sure there was enough work for him.
Pretty soon, it became clear that there was, in fact, plenty of work in International Falls, Minn., a town of 6,000 people. He split his time between a group family practice and community mental health center and also saw patients in nearby communities.
“Within two or three years, it was clear I was too busy to go out of town anymore,” he said.
After nearly 30 years working as the town’s sole psychiatrist, Hardwig retired in September, leaving no psychiatrists for more than 100 miles around. His departure underscores a difficult reality: A national shortage of psychiatrists is much more acute in rural and remote areas, which leaves many people without access to the kind of services they need.
And the demand for Hardwig’s services has never let up.
Wendy Dougherty, the nurse who worked with him at the clinic, said his calendar was always full.
“He never ever … in the five years I worked with him, ever had an empty slot,” she said. “And one thing about his patients, if they called and canceled, that empty slot was filled by somebody that had been waiting two months to get in.”
But, she said, he was also the kind of doctor who would always find a way to squeeze in somebody in a crisis, even if it meant missing lunch or canceling his own meetings.
‘You take all comers’
The clinic where Hardwig worked is a primary care center on the outskirts of town, part of the Duluth-based Essentia Health system. It’s a low-slung building across the street from a Menards and a Dollar Tree that offers all the basic services, including annual checkups and mammograms.
Hardwig and others agree that the need for a psychiatrist in town was there, but until he arrived, people mostly counted on their primary care doctors to handle it.
His patients’ diagnoses over the years ran the spectrum of diseases, including anxiety, depression, bipolar disorder and schizophrenia.
“I had to take care of people of all ages — all the way through to the nursing home,” he said. “You can’t really specialize if you’re in a small town. You take all comers.”
And working in a small town, he also couldn’t avoid running into his patients frequently. It might have been hard for some doctors — psychiatry is a profession that particularly prizes its discretion — but Hardwig says he didn’t mind.
“I just had sort of an agreement with my patients if they say ‘hi’ to me, I’ll say ‘hi’ back, but I won’t otherwise out them. And my wife knew not to ask, ‘How do you know that person?’” he said.
He said his patients were respectful of him, too, and didn’t try to squeeze in consultations in line at the grocery store or when he was out to dinner.
One of his longtime patients was a man named Daniel Carr, whom I met at a clubhouse run by a community mental health center where people with serious mental illness can spend their time. The cozy house has battered couches and an armchair in the living room. A Christmas tree sparkles near the front window.
Carr, who has paranoid schizophrenia, was Hardwig’s patient for 25 years. He says he misses Hardwig.
“He knew exactly about how to treat me,” Carr said.
“I had some trouble with my medicine changing a little one way or the other, but he usually knew what was best. I’d tell him what I was experiencing and he knew what to do.”
Hardwig wouldn’t talk about specific patients, including Carr. Carr said his psychiatric care has been transferred back to his primary care doctor, and that it’s been going OK so far.
But Wendy Dougherty, the nurse who worked with Hardwig, said some of the primary care doctors have been less than enthusiastic about taking on the psychiatrist role.
“Jeff took care of the hard ones,” she said. “The schizophrenics, the bipolars … these docs kind of put up their hands and say, ‘Oh, my God, I don’t know what meds to give them.’”
The psychiatric nurse practitioner Hardwig worked with is still at the clinic and handles some of the harder cases, but she’s planning to retire soon, too.
A shortage in nearly every county
International Falls is hardly alone in not having a psychiatrist — particularly in remote areas.
More than 90 percent of psychiatrists only work in urban areas, even though more than 20 percent of Americans live in rural areas. In Minnesota, nearly every county — aside from the Twin Cities metro and Rochester area — is considered to have a shortage of mental-health professionals as determined by federal guidelines.
Hardwig said the hardest part of working in such a remote area was that he didn’t have a continuum of care to work with.
“There just isn’t that inpatient bed when you need it. We have only one crisis bed and we haven’t had that the whole time I’ve lived here. We don’t have residential treatment,” he said.
And International Falls is luckier than some places because there’s a community mental health clinic in town. (Hardwig partnered with it until his retirement, and the nurse practitioner still does.) The clinic is looking to expand in the near future. There’s also a mobile crisis team in town that can help with emergencies.
Still, recruiting mental-health care providers, even those who aren’t psychiatrists, to remote areas is challenging. Paul Mackie, a professor at Minnesota State University, Mankato, has studied the problem. And he said the only way to recruit and retain people in remote areas is to grow them from scratch. That is how Hardwig, who grew up in International Falls, ended up there.
Mackie said there are already physical medicine programs that train people for practice in rural areas. And he said now we need to do the same for mental health, too.
“We need to be a lot more thoughtful about who we’re recruiting and how we’re recruiting them,” he said. “We can have that conversation around what does a rural practitioner look like and look for that person and encourage them.”
But that takes time. People who graduated from high school this year won’t be done with medical school until 2027. And then they still have to complete their residency and any other specialty training.
So in the meantime, International Falls — and communities like it — are doing what they can. Hardwig’s old clinic has hired a child psychiatrist who sees her patients remotely over Skype-like technology.
Finding people to work on-site is proving much trickier, though. It was two years ago that Hardwig told the clinic he was planning to retire. It’s been looking for a replacement since then. But nobody has applied for the job.
Holiday Tips
I recently saw a meme on social media that said “It’s almost time for my normal anxiety to turn into my fancy holiday anxiety.” I had to chuckle when picturing anxiety showing up in a glittery ugly sweater or draped in all things sparkly. Humor aside, it shows that during the holidays, our existing anxiety (or depression) does not just “take a holiday” but rather increases due to stress and societal pressures.
This time of year can be an incredibly stressful and frustrating time. On one hand, we fill our days to the brim with spending time with family and friends, social events, potlucks, baking, preparing meals, finding the right present within your means, and many other tasks guised in the name of the holidays. All of this “fun” can turn to chaotic quickly. Then on the other hand, some of us may have unwelcome reminders or memories associated with the holidays or feel more alone during this time as we watch others join together and celebrate. Whatever the reason for your distress, here are some helpful strategies to help manage the rise of our fancy anxiety (or depression) in finding ways to relax during the busy time of year or help with our perspective on the season.
- Self-soothe – Using all 5 senses, focus on what you notice. Cast any judgments away and focus on the experience in the moment. Here are some examples.
- Taste – slowly eat and notice different flavors in a favorite holiday treat or dish
- Smell – light a candle or smell a pine tree or cup of tea
- Sound – listen to your favorite holiday music, point our different instruments or lyrics you might have over looked
- Sight – watch the fireplace flicker with light or notice the holiday lights all around
- Touch – when baking or wrapping gifts, bring attention to the different textures you feel
- Pay it forward – doing something kind for others or contributing can make us feel good about ourselves and give perspective. This could be anything from holding a door open for someone, greeting someone with a smile, adopting a family for the holiday, or volunteering. It does not need to be a large act to bring a sense of contribution to your holiday.
- Be intentional about breaks – Set aside 15 minutes to check in with yourself and pause from all of the holiday excitement. Read a favorite book, do a meditation, sit in silence, or snuggle up with someone you love.
- Simplify and slow down – With your to-do list growing, it may feel like you need to be in multiple places at once; however, what we know about the brain is that it cannot think 2 things at once. So, focus your entire attention to the task at hand rather than jumping from task to task (aka multitasking).
- Follow traditions (or make your own new ones) – Partake in something that brings you meaning for the season, whether this be a family tradition, baking Grandma’s cookies, or finding something new to do this time of year (i.e., sledding, ice skating, driving around to see holiday lights, etc).
- Put down the phones – I know, I said it. Just hear me out. Often times social media can impact our level of stress by comparing ourselves to others, especially when those others seem to have it all together. They have the catalog ready decorations, Martha Stewarts holiday food spread, or gifts we cannot afford. This can lead us into a down spiral. So, try to limit your access to your phone and engage with those around you.
- Reach out to someone– The holidays can be a lonely time for some. Sometimes we can still feel lonely in a room full of people, feel so far away and disconnected from others, or feel forgotten. Use all of your willingness to reach out to someone or connect. Whether that be grabbing a cup of hot cocoa with a friend, attending a service, volunteering, or making a phone call to someone you have lost touch with in the past. We are social creatures and need human connection.
- Be real with yourself – This includes preparing to spend time with family or friends. You likely already know who is going to be the Grinch, who is going to over indulge in the holiday punch, who is going to bring up politics, and who is going to ask about your love life. Just because it is the holidays, does not mean we are going to change who we are or the roles we play. Have an action plan for how you are going to deal with the likely interactions or dynamics.
- Life in moderation – Life is about balance. Enjoy the holidays by partaking in the indulgences and socialization. Moderation is key. Listen to your body and the signals it is giving you.
- Gratitude– Research is growing on the importance and efficacy of practicing gratitude in daily life. Our brains are inherently negative so being intentional about shifting out of the holiday stress (and negativity) can help bring perspective and renew our enjoyment of the season.
- Write down things you are thankful for in life. Focus on the small things (i.e., clean water, fresh air, etc). Nothing is too small to be grateful for in life.
- Reflect one thing you believe you did well over the past year.
- Compare yourself to a time in your past when you might have handled the holiday stress less effectively.
- Permission grant yourself – The holidays are not always candy canes and sprinkles. Often times we hold ourselves to high expectations and forget we are in control of our own actions. Grant yourself permission to: take time outs/breaks, have fun, do things “out of order”, celebrate differently than family/friends/the past, start a project and stop, be honest with people (and yourself), or have days that are “humbug” or just okay.
Feel free to make these tips your own by adding your own personal flair to them. It is important to find what works for you and your fancy holiday distress.
Happy holidays,
Dr. Alison Dolan
7 Ways Loneliness (and Connectedness) Affect Mental Health
Loneliness is finally starting to get at least some of the attention it deserves—we may not be as “on it” as other countries, like the U.K. with its Minister for Loneliness, but we’re getting there. Like the push to dissolve the stigma around mental health issues, there’s been a similar increase in people’s honesty about their social connection, or lack thereof. And it turns out that people are pretty lonely these days. The percentage of people saying they have few or no confidants has risen precipitously in recent years. So if you’re feeling lonely, you’re…well, not alone.
As the research shows just how important social connection is for our health and mental health, and how detrimental loneliness can be, the value of speaking out—and changing our habits—becomes all the more clear. Here are some of the ways in which loneliness hurts us and social connectivity helps us, psychologically and physiologically.
Loneliness is contagious
Other work has shown that people who become lonelier over time also begin to trust others less, which creates a vicious cycle of loneliness and social isolation. These types of studies suggest that social connection is precarious, and vulnerable to different forces, making it all the more important to do what we can to keep our networks together and oneself involved.
Past Trauma May Haunt Your Future Health
Adverse childhood experiences, in particular, are linked to chronic health conditions.
A rocky childhood. A violent assault. A car accident. If these are in your past, they could be affecting your present health.
These are all examples of traumatic events — which, in psychological terms, are incidents that make you believe you are in danger of being seriously injured or losing your life, says Andrea Roberts, a research scientist with the Harvard T.H. Chan School of Public Health. Research shows that these events can trigger emotional and even physical reactions that can make you more prone to a number of different health conditions, including heart attack, stroke, obesity, diabetes, and cancer.
Understanding trauma
Traumatic events encompass anything from a sexual assault or childhood abuse to a cancer diagnosis. Child abuse is particularly likely to affect your adult life because it occurs at a time when your brain is vulnerable — and it often occurs at the hands of people who are supposed to be your protectors, says Roberts. “By abuse, we often mean things that are a lot milder than things people typically think of as abuse. It might include being hit with a hard object, like a whip, a belt, or a paddle,” says Roberts. “The behavior doesn’t necessarily need to be illegal to induce a traumatic response.”
A child’s perception of events is as important as what actually occurred. “While a child’s life may not have actually been in danger, the child may have seen it as life-threatening,” says Dr. Kerry Ressler, a psychiatry professor at Harvard Medical School.
People who experience traumatic events sometimes develop post-traumatic stress disorder (PTSD), a psychiatric condition that affects 5% to 10% of the general population, says Dr. Ressler. It’s more common in women, affecting twice as many women as men. And it also occurs more frequently in people who have certain risk factors, including those living in poverty, soldiers in active combat, and first responders, he says. PTSD can develop after a person experiences violence or the threat of violence, including sexual violence. It may affect people who have a close relative who experienced those things as well, says Dr. Ressler. These traumatic events are generally incidents that are considered outside the ordinary and are exceptional in their intensity.
Exposure and risk
Your risk for mental and physical health problems from a past trauma goes up with the number of these events you’ve experienced. For example, your risk for problems is much higher if you’ve had three or more negative experiences, called adverse childhood experiences (ACEs), says Roberts.
These include
- physical abuse
- sexual abuse
- emotional abuse
- physical neglect
- emotional neglect
- witnessing domestic violence
- substance misuse within the household
- mental illness within the household
- parental separation or divorce
- incarceration of a household member.
Another kind of trauma
While severely traumatic events are believed to have the greatest effect on long-term health, other stressful events that don’t necessarily meet the psychological definition of trauma can still cause problems. This might include a sudden death in the family, a stressful divorce, or caring for someone with a chronic or debilitating illness, says Roberts. These milder events might lead to a mental health disorder, such as anxiety or depression. “Trauma pushes your ability to cope, so if you have a predisposition toward anxiety, for example, it may push you over the edge,” says Roberts.
In addition, incidents like these can also produce PTSD-like symptoms in certain people. “When people go through traumatic or complicated grief, they can experience pretty similar symptoms to those they might experience with trauma, such as intrusive thoughts,” says Dr. Ressler.
Medical conditions resulting from trauma
Most of the research related to trauma and chronic disease risk has focused on childhood trauma, says Dr. Ressler. Early childhood trauma is a risk factor for almost everything, from adult depression to PTSD and most psychiatric disorders, as well as a host of medical problems, including cardiovascular problems such as heart attack and stroke, cancer, and obesity.
These effects likely reflect two factors:
Behavioral changes resulting from trauma. People who are suffering from traumatic memories may try to escape them by participating in risky behaviors such as drinking, smoking, drug use, or even overeating for comfort. “Those can all be used as a coping mechanism, a way of dealing with emotional dysregulation that occurs when someone has been traumatized,” says Roberts. These habits, in turn, lead to health problems.
Physical effects related to trauma. The problem goes beyond unhealthy habits. Experts believe that there is actually a direct biological effect that occurs when your body undergoes extreme stress. When you experience something anxiety-provoking, your stress response activates. Your body produces more adrenaline, your heart races, and your body primes itself to react, says Roberts. Someone who has experienced trauma may have stronger surges of adrenaline and experience them more often than someone who has not had the same history. This causes wear and tear on the body — just as it would in a car where the engine was constantly revving and racing, she says. Stress responses have also been demonstrated in people who have experienced discrimination throughout their lives. “It ages your system faster,” says Roberts.
Chronic stress can increase inflammation in the body, and inflammation has been associated with a broad range of illness, including cardiovascular disease and autoimmune diseases, says Roberts. Early trauma disrupts the inflammatory system. This can lead to long-term aberrations in this system and chronic health problems triggered by constant inflammation. Typically, the more trauma you’ve experienced, the worse your health is.
Barriers to getting help
People who have experienced trauma may also struggle with getting help. “One of the most common outcomes of trauma is avoidance,” says Dr. Ressler. “It makes sense. If you experience something traumatic, you want to avoid thinking about it and going to places that remind you of it.” Unfortunately, health settings — with their doctors, therapists, and counselors — are triggers for many people because when someone experiences a traumatic event, he or she often ends up in the health care system.
In addition, if you’ve experienced trauma, you may believe that health care providers will want you to talk about it and dredge up feelings from the past. For these reasons, people who have experienced trauma may avoid medical care.
Some people may be in denial about the role past trauma is playing in their life. “I would say that a lot of people are unaware of how trauma is affecting them,” says Roberts. One of the hallmarks of trauma is the fact that people often use defense mechanisms to protect themselves from stress. Denial is one of those, as is trying to normalize past problems. “People may say things like, ‘oh, everybody I know got hit as a child,'” says Roberts.
Seek out resourcesTo get more information about trauma and PTSD or to find treatment resources, here are three very good, well-vetted websites from leading professional organizations:
|
Getting help
If you suspect that past trauma is affecting your life, there is help. This is a treatable problem. “You don’t have to be stuck,” says Dr. Ressler. “There is a good chance that you can move past this.”
Taking steps to address the problem may also help others in your life. Very often people who have experienced trauma pass problems on to others in their family through a process called observational learning, he says. So, helping yourself may help those around you. Consider these steps.
Work with a therapist. A trained therapist can help you reframe what happened to you and help you move past it. “One of the most successful treatments is exposure therapy, where the idea is to expose yourself in small doses to the thing that was most traumatizing, with someone there to support you,” says Roberts. Treatment may also include medication to address any mental health disorders you are experiencing.
Take care of yourself. There are numerous lifestyle measures that can help you reduce stress and anxiety. These include yoga, tai chi, and meditation. Regular exercise can also help you manage stress and other symptoms.
Reach out to others. Research has shown that maintaining strong social ties with friends and family members is crucial to good mental health.
“Unfortunately, all of these things are hard to do when in depressive states,” says Roberts.
That’s why many people may need to start with therapy, and then add other strategies later on.
How to Address Your Teen’s Issues with Poor Motivation
Getting your teen to improve his or her focus.
“If the eye is patient enough, it will get a clear view of the nose.” – Anonymous
When people think about issues related to poor concentration, they immediately think about distractions. This is even more the case when it concerns teens. Things that come to the mind of the casual observer, are smart phones, social media and troubled peers.
A quick Google search for how to improve your teen’s lack of focus, will bring up issues like attention deficit hyperactivity disorder (ADHD/ADD), depression, nutrition and strategies for developing a more efficient schedule. These topics and recommended strategies are appropriate and effective for helping your teen improve his or her issues with focus, but they cannot be effectively applied until one important issue is addressed.
Motivation.
That’s right. The primary reason young people struggle with poor focus and concentration is a general lack of motivation to do anything meaningful. The teen who lacks motivation will often gravitate towards activities which greatly stimulate neuro-chemicals associated with the brain’s reward system.
Activities such as video games, food, mind altering substances, alcohol and sex. These are things bored teens are likely to engage in habitually, in order to feel alive. This is because, in the absence of motivation to succeed, the teen is faced with a difficult reality consisting of a monotonous chore and a daily schedule. Even things like daily showers can seem time consuming and tiring to a teen who struggles with low motivation. It is also important to note that these issues are also symptoms of depression with a teen.
Before we begin processing on how to get teens more motivated, it is important to come to an understanding on what motivation is. According to Wikipedia, the term motivation is derived from motive. Motive means a need that desires satisfaction. So, for a teen to be motivated, he or she must be actively pursuing a need which desires satisfaction.
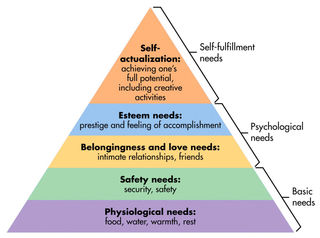
Maslow’s Hierarchy of Needs.
Typically, we understand needs to be intrinsic materials necessary to keep us alive, such as food, water and shelter. However, an expanded discussion on the issue of needs would be based on the famous work of Abraham Maslow, regarding his hierarchy of emotional needs.
According to Dr. Maslow’s theory, there are two types of needs people strive for. They are deficiency needs and growth needs. Deficiency needs are comprised of basic needs and psychological needs. These are physiological needs, which have to do with food, water and shelter. Followed by the need for safety and security. The physiological needs and the safety needs are known as basic needs.
Next are the psychological needs, which have to do with the needs for a sense of belonging and feeling accepted. This is also followed by the need for esteem, which has to do with prestige and status in society. According to Dr. Maslow, people are only motivated to get these needs met, when these needs are deficient in their lives. Once these needs are met, people are no longer motivated in getting them met, which opens the door for addressing growth needs.
Then there are the self-fulfillment needs, which Dr. Maslow describes as self-actualization coming from having achieved one’s full potential. He also describes this as growth needs. Unlike deficiency needs, people become more motivated as their growth needs are met.
So, a teen who practices the courage to do his best in understanding calculus, becomes more motivated the more he succeeds and subsequently more focused. Further, teens who are experiencing success in achieving their potential, are also very disciplined in their home life. For example, they are disciplined in following through consistently with their assigned chores and personal hygiene.
It has been theorized that teens who struggle with depression, have experienced very little success in effectively getting their psychological needs met. This topic will be addressed in another post.
Often Motivated.
Upon examining Maslow’s hierarchy of needs, it is easy to conclude that most teens don’t have low motivation. Rather, most teens are preoccupied to getting their deficiency needs (acceptance and recognition) met, rather than their growth needs (success in academia) met.
Such a phenomenon is easy to witness with teens from low socio-economic backgrounds, such as an obsession in getting their physiological and safety needs met. However, with teens from middle class backgrounds and up, their focus is often on their psychological needs. For example, relationship with friends, close friendships and status among peers.
When teens are focused on getting their deficiency needs met, they are not going to be focused on issues regarding self-discipline and mastery. For a parent to help his or her teen become more focused on growth needs, he or she will have to teach his or her teen how to effectively get their deficiency needs met.
Conflict of Beliefs and Values.
This may be easier said than done, as today’s teenager is often exposed to new values and beliefs through social media. Meaning, that these values and beliefs are often in conflict with the teaching of the parents.
So, efforts to help the teen address his or her deficiency needs may result in a stalemate between parent and teen. Which then leads to a recurring problem with a lack of focus due to poor motivation with issues like school work, personal hygiene and chores.
The solution for a situation like this will be for parents to seek therapeutic services to assist their teen in effectively getting their deficiency needs met, in order to focus on his or her growth needs.



