Acknowledging Your Anxiety
I’ve been talking with my clients a lot recently about how to manage anxiety and stress. We’re all experiencing probably a higher level of anxiety than what we’re used to. Some people have a lot of skills for managing that and some of us don’t
Creating Social Connections through Quarantine
Our need for human connection is so powerful that it is essential to our physical and mental well-being.
How to Transition From In-Person to Online Therapy During Coronavirus
How to Transition From In-Person to Online Therapy During Coronavirus
To help prevent the spread of the coronavirus, the Centers for Disease Control and Prevention (CDC) recommends social distancing. This means that individuals are encouraged to limit unnecessary social contact.
In response, many people are changing the way they conduct business—including therapists. Meeting with a therapist might place both you and the therapist at a higher risk of catching (and spreading) the virus. In addition, any other staff members or patients you come in contact with in the waiting room may also increase the risk that the virus will be spread.
To reduce in-person contact, some therapists are starting to offer online treatment. Whether meeting via video or phone, virtual therapy appointments aren’t the same as meeting face-to-face, so it’s important to educate yourself about what to expect and how it may impact your treatment.
Differences Between In-Person and Online Treatment
There are some big differences between online therapy and face-to-face therapy. And while online treatment can be convenient for some people—especially during the coronavirus pandemic—it does have some potential drawbacks.
Keeping the Same Therapist
If you’re already attending therapy, you may want to ask your therapist about any virtual treatment options if you’re concerned about social distancing. Your therapist, of course, may bring it up first as well.
But before agreeing to do it, it’s important to consider how your treatment may change if you aren’t meeting face-to-face.
Ask how your therapist will be providing treatment. Will you speak over the phone? Can you communicate via video chat? Can you send emails or messages?
Have a conversation about any concerns you may have. Discuss what you’ll do if you run into any obstacles while trying to conduct online therapy. You may encounter practical problems, like technical glitches, or you may discover that either your progress slows or your appointments don’t seem to be as effective.
Having a candid discussion about the obstacles you might encounter as well as how you can address issues if they arise can be very helpful. When you have a plan in place, you’ll feel more confident about your ability to make the best of online therapy.
Remember, there’s always a chance you might even like online or phone therapy better than face-to-face therapy.
After all, you’ll spend less time commuting to appointments. Your therapist may also offer more flexible hours. And you may even find that it’s easier to be more forthcoming with information when not in the same room as your therapist.
Body Language
Another factor to consider if you’re going to meet online is your body language. During face-to-face treatment, you and your therapist can read one another’s body language.
This is much tougher to do during video chats, and it’s impossible to do if you’re talking over the phone. You might find it’s difficult to know how your therapist is responding if you can’t see their body language or facial gestures.
On the flipside, your therapist won’t be able to read your body language either. When you say that you’re doing “fine,” do you really mean fine? Perhaps your body language says something different. Without being in the same room, your therapist may be more likely to miss vital visual clues about your emotional state.
Not all Types of Therapy Work Well Online
Many forms of talk therapy can work over the phone, via email, or video chat. But some types of treatment just aren’t made for virtual sessions.
Sand tray therapy and EMDR, for example, may be challenging to do virtually. So you’ll want to talk to your therapist about the type of treatment you’re receiving and whether it will still work online or over the phone.
Getting a New Therapist
Not all therapists are equipped to offer virtual appointments. Some of them may be uncomfortable conducting phone therapy. Others may not have the means to provide secure, confidential email or video chat services.
If your therapist isn’t able to provide virtual treatment, you might decide to seek treatment with a new therapist. It can be helpful to talk to your in-person therapist about this.
Ask your therapist if they think you’re a good candidate for online therapy. Individuals with serious mental illnesses or people with suicidal ideation, for example, are typically not good candidates for online therapy.
Your therapist can help you decide if virtual treatment is right for you. Discuss any mental health diagnoses or pertinent information that you’d want to share in online therapy. And review how you can continue to make progress with a new therapist while using a new form of treatment.
Do a little research to learn about the different online therapy options. Consider what type of communication you might want to use—video chats, text messaging, or phone calls. Explore prices and various online options so you can make an informed decision about which online service you think will best meet your needs.
Questions to Ask Your Therapist Before Beginning Treatment
Before you transition to online therapy, it’s important to ask questions about your treatment. Here are some things you may want to address:
- How will I sign the paperwork? Does your therapist have a way for you to electronically sign forms, like treatment plans or consent forms?
- How is my information kept confidential? Any video chat service or email messaging service you use must meet specific regulations to ensure that your information is kept safe and confidential.
- Does my insurance cover this? Most insurance companies do not cover online treatment. So you’ll want to ask your therapist whether they accept insurance. You may also want to contact your insurance company to learn about your options.
- How much will it cost? Online therapy typically costs less than in-person treatment. But if you’re transitioning to online therapy with a therapist you’ve been seeing, the price may not necessarily change.
- What type of technology do I need? Ask about whether you’ll need to download any apps or software. Also, find out if you can video chat from mobile devices or whether you’ll need a computer.
Coronavirus Related Issues You May Want to Address
If you’re meeting with a therapist online because you’re social distancing, you may have coronavirus-related issues to address.
Here are some examples:
- How can I manage my mental health when I’ve reduced my social contact?
- What can I do about my anxiety surrounding the coronavirus?
- Now that I’m spending more time at home, what steps do I need to take to stay as mentally healthy as possible?
- Are there specific exercises or strategies I can use to build mental strength?
- How should I talk to my kids about the coronavirus?
- What can I do about my financial stress during this time?
7 Tips to Make the Most of Online Therapy During the COVID-19 Outbreak
7 Tips to Make the Most of Online Therapy During the COVID-19 Outbreak
A couple of years ago — long before COVID-19 was an unfortunate glimmer in the CDC’s eye — I made the decision to switch from in-person therapy to telemedicine.
As someone who has historically struggled with opening up to therapists, my hope was that I would find it easier to be vulnerable if I could hide behind a screen. What I found was that I was able to disclose more, and as a result, it deepened the therapeutic relationship.
Not only did this transform my therapy experience — it also unwittingly prepared me for the huge shift to telehealth that’s now happening in light of the recent COVID-19 outbreak.
If you’re looking to start online therapy, or if your therapist has moved their practice to digital for the unforeseeable future, it can be a jarring transition.
While it can be a big adjustment, online therapy can be an amazing and worthwhile support system — particularly in a time of crisis.
So how do you make the most of it? Consider these 7 tips as you make your transition to teletherapy.
1. Carve out a safe space and intentional time for therapy
One of the most touted benefits of online therapy is the fact that you can do it any time, anywhere. That said, I don’t necessarily recommend that approach if you can avoid it.
For one, distractions are never ideal when you’re trying to work — and therapy is rigorous, difficult work sometimes!
The emotional nature of therapy makes it even more important to have some space and time set aside to engage with this process fully.
If you’re self-isolating with another person, you could also ask them to wear headphones or take a walk outside while you do therapy. You might also get creative and create a blanket fort with string lights for a more soothing, contained environment.
No matter what you decide, make sure you’re prioritizing therapy and doing it in an environment that feels safest for you.
2. Expect some awkwardness at first
No matter what platform your therapist is using and how tech-savvy they are, it’s still going to be a different experience from in-person — so don’t be alarmed if it doesn’t feel like you and your therapist are “in-sync” right away.
For example, when my therapist and I used messaging as our primary mode of communication, it took some time for me to get used to not being replied to right away.
It can be tempting to think that some discomfort or awkwardness is a sign that online therapy isn’t working for you, but if you can keep an open line of communication with your therapist, you might be surprised by your ability to adapt!
It’s also normal to “grieve” the loss of in-person support, especially if you and your therapist have worked together offline before.
It’s understandable that there could be frustration, fear, and sadness from the loss of this type of connection. These are all things that you can mention to your therapist as well.
3. Be flexible with the format of your therapy
Some therapy platforms use a combination of messaging, audio, and video, while others are a typical session over webcam. If you have options, it’s worth exploring what combination of text, audio, and video works best for you.
For example, if you’re self-isolated with your family, you may rely on messaging more frequently as not to be overheard by someone and have as much time as you need to write it. Or if you’re burnt out from working remotely and staring at a screen, recording an audio message may feel better for you.
One of the benefits of teletherapy is that you have a lot of different tools at your disposal. Be open to experimenting!
4. Lean into the unique parts of telemedicine
There are some things you can do with online therapy that you can’t necessarily do in-person.
For example, I can’t bring my cats to an in-person therapy session — but it’s been special to introduce my therapist to my furry companions over webcam.
Because online therapy is accessible in a different way, there are unique things you can do to integrate it into your daily life.
I like to send my therapist articles that have resonated with me for us to talk about later, set up small daily check-ins instead of just once weekly, and I’ve shared written gratitude lists over text during especially stressful times.
Getting creative with how you use the tools available to you can make online therapy feel a lot more engaging.
5. In the absence of bodily cues, practice naming your emotions more explicitly
If you’ve been in in-person therapy for a while, you may be used to your therapist observing your bodily cues and facial expressions, and sort of “intuiting” your emotional state.
Our therapists’ ability to read us is something we might take for granted as we pivot to telemedicine.
This is why it can be really beneficial to practice naming our emotions and reactions more explicitly.
For instance, if your therapist says something that strikes a nerve, it can be powerful to pause and say, “When you shared that with me, I found myself feeling frustrated.”
Similarly, learning to be more descriptive around our emotions can give our therapists useful information in the work that we do.
Rather than saying “I’m tired,” we might say “I’m drained/burnt out.” Instead of saying “I’m feeling down,” we might say, “I’m feeling a mix of anxiety and helplessness.”
These are useful skills in self-awareness regardless, but online therapy is a great excuse to start flexing those muscles in a safe environment.
6. Be willing to name what you need — even if it seems ‘silly’
With COVID-19 in particular, an active pandemic means that many of us — if not all — are struggling with getting some of our most fundamental human needs met.
Whether that’s remembering to eat and drink water consistently, grappling with loneliness, or being fearful for yourself or loved ones, this is a difficult time to be a “grownup.”
Taking care of ourselves is going to be a challenge at times.
It can be tempting to invalidate our responses to COVID-19 as being an “overreaction,” which can make us reluctant to disclose or ask for help.
However, your therapist is working with clients every day who undoubtedly share your feelings and struggles. You aren’t alone.
What should I say?
Some things that might be helpful to bring to your therapist during this time:
- Can we brainstorm some ways to help me stay connected to other people?
- I keep forgetting to eat. Can I send a message at the beginning of the day with my meal plan for the day?
- I think I just had my first panic attack. Could you share some resources for how to cope?
- I can’t stop thinking about the coronavirus. What can I do to redirect my thoughts?
- Do you think my anxiety around this makes sense, or does it feel disproportionate?
- The person I’m quarantined with is impacting my mental health. How can I stay safe?
Remember that there’s no issue too big or too small to bring to your therapist. Anything that’s impacting you is worth talking about, even if it might seem trivial to someone else.
7. Don’t be afraid to give your therapist feedback
A lot of therapists who are making the shift to telemedicine are relatively new to it, which means there will almost certainly be hiccups along the way.
Online therapy itself is a more recent development in the field, and not all clinicians have proper training on how to translate their in-person work to a digital platform.
I don’t say this to undermine your faith in them — but rather, to remind and encourage you to be your own best advocate in this process.
So if a platform is cumbersome to use? Let them know! If you’re finding that their written messages aren’t helpful or that they feel too generic? Tell them that, too.
As you both experiment with online therapy, feedback is essential to figuring out what does and doesn’t work for you.
So if you can, keep communication open and transparent. You might even set aside dedicated time each session to discuss the transition, and what has and hasn’t felt supportive for you.
Online therapy can be a powerful tool for your mental health, especially during such an isolating, stressful time.
Don’t be afraid to try something different, vocalize what you need and expect, and be willing to meet your therapist halfway as you do this work together.
Now more than ever, we need to protect our mental health. And for me? I’ve found no greater ally in that work than my online therapist.
Weekly Intervention Ideas: March 30th Edition
Weekly Intervention Ideas: March 30th Edition
Kid strategy of the week:
- Video: Inside Out: Guess the Feelings
- Scavenger Hunt: have the child search around the house for these items and share them with you:

Couples strategy of the week:
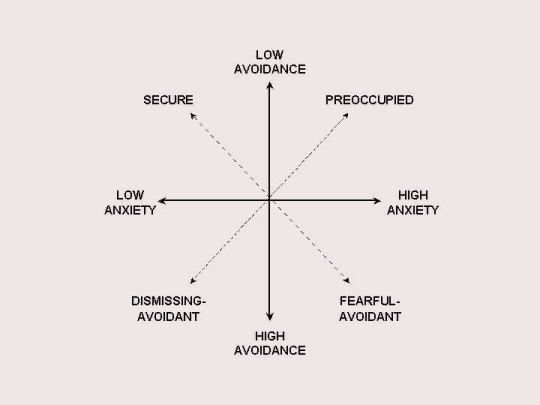
- Help couples figure out similarities and differences in their attachment styles, and process how their attachment styles may play impact their relationship dynamics.
- Attachment Styles Assessment: https://dianepooleheller.com/attachment-test/
- Video: https://www.youtube.com/watch?v=2s9ACDMcpjA
Adult strategy of the week:
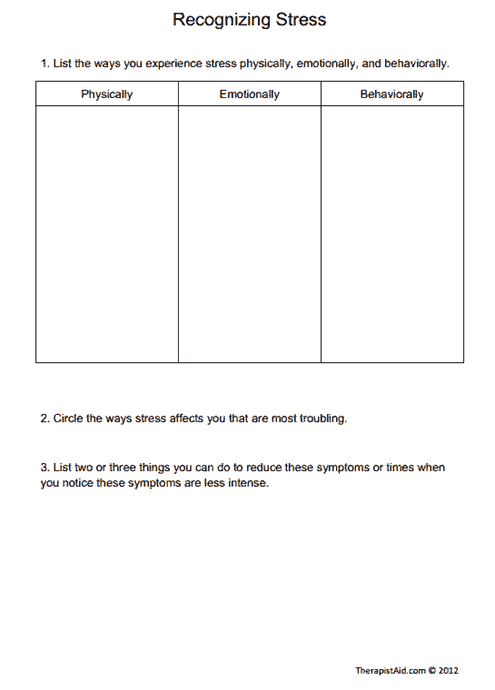
- Many people are experiencing high levels of stress right now. Sometimes, we are not even aware of the ways that our bodies and minds are reacting to stress. Use this worksheet to recognize signs of stress and discuss coping strategies for reducing stress and establishing healthy coping strategies
- https://www.therapistaid.com/worksheets/recognizing-stress.pdf
Five Secrets to Calming Yourself
Mindfulness/Meditation of the week:
● Loving Kindness Meditation
This loving kindness practice involves silently repeating phrases that offer good qualities to oneself and to others.
Let’s begin by settling into a comfortable position, whatever feels right for your body. Bring attention to your breath. Notice the still points between your breaths. Breathe in through the nose to the count of 4 and out to the count of 6. Focusing on the still place between breaths.
- Now shifting attention to our thoughts. Begin by taking delight in your own goodness—calling to mind things you have done out of good-heartedness, and rejoicing in those memories to celebrate the potential for goodness we all share.
- Silently recite a phrase that reflects what we wish most deeply for ourselves in an enduring way. Some examples are:
• May I live in safety.
• May I have mental peace
• May I have physical health
• May I live with ease. - Repeat a phrase with enough space and silence between breaths so they fall into a rhythm that is pleasing to you. Directing your attention to one phrase and breath at a time.
- Each time you notice your attention has wandered, be kind to yourself and let go of the distraction. Come back to repeating the phrase without judgment.
- (Few more breaths) … now, visualize yourself in the center of a circle composed of those who have been kind to you, or have inspired you because of their love. Perhaps you’ve met them, or read about them; perhaps they live now, or have existed historically or even mythically. That is the circle. As you visualize yourself in the center of it, experience yourself as the recipient of their love and attention. Keep gently repeating the phrase of loving kindness for yourself.
(few breaths) Slowly transitioning out of the visualization, and simply keep repeating the phrases for a few more breaths. Each time you do so, you are transforming your old relationship to yourself, and are moving forward, sustained by the force of kindness and compassion inward.
Mindfulness in the Midst of a Pandemic
As a therapist, people tend to look to me for answers. We ask the questions to gain understanding and help guide and walk with people on their journeys. In the midst of a pandemic, how does that work though?
Pandemic-Related Anxiety
Feelings of increased stress, anxiety, and depression are now a new “normal baseline” for a population finding themselves faced with fear and uncertainty.
6 Ways to Manage Anxiety During The Coronavirus Outbreak
Everyone has been talking about the Coronavirus, otherwise known as COVID-19. It’s all over the news, it’s pervading daily conversation, and it’s supposedly pretty scary for our older population, particularly those with underlying severe, chronic health conditions. This global epidemic (and some may call it a full-fledged pandemic) is impacting our global health, economy and way of life as we know it.
According to the World Health Organization (WHO), “Coronaviruses (CoV) are a large family of viruses that cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS-CoV). A novel coronavirus (nCoV) is a new strain that has not been previously identified in humans.”
Common signs mimic a common cold or flu, with respiratory symptoms such as a cough, fever, shortness of breath or trouble breathing.
As more and more confirmed cases start popping up all around us, anxiety naturally increases.
WHAT IS ANXIETY?
Anxiety is like worry on caffeine. Anxiety is our brain’s way of letting us know that something is unsafe, dangerous or potentially harmful/deadly. We are survival creatures and we don’t like things to disrupt our safe, consistent routine. COVID-19 has begun to do just that.
Anxiety is adaptive. If we sense danger (even perceived danger), our brain perks up and gets our body ready for action to fight, run or freeze. This is how we protect ourselves and those we love.
Anxiety is only good until a certain level. Because anxiety motivates us and keeps us safe, it works great for short bursts and for specific situations. What happens when we are overly anxious for too long of a time? It’s different for everyone, but if we are too anxious, it no longer helps us, and it can begin to interfere with our daily life. We may be recluses, avoid, become depressed or even develop panic attacks.
When we enter an unknown situation like a global viral epidemic, fears run wild. We have little past experience on what to expect, how things may change (humans hate change!) and the future impact on our health – physically, emotionally, financially and economically.
We must have anxiety during this time, as it helps us become prepared to take on a threat to our existence. Yet, we still don’t know what will become in our country or in our state. For our own mental health and the mental health of our children watching how we react and respond…we must find ways to use both our emotion mind and our logic mind to stay in the WISE mind (to learn more about “wise mind”, look up Dialectical Behavior Therapy- DBT).
6 WAYS TO MANAGE ANXIETY DURING THE CORONAVIRUS (COVID-19) OUTBREAK
REDUCE YOUR PREOCCUPATION WITH CORONAVIRUS NEWS
Coronavirus is undeniably a major topic of discussion in the news, but constantly listening to updates and reading stories may lead to increased anxiety. It’s also important to know which news sources are providing accurate information so you’re not distressed over news that isn’t even factual. Limit your news consumption so you can stay informed without becoming preoccupied. The WHO is a great resources as is the CDC.
Turn off the t.v. when enjoying a family meal. Turn off alerts from news outlets on your phone. Set aside one or two times a day (if needed) to look at credible news sources so that you can function throughout the rest of your day at school, work or at home.
KNOW YOUR OWN RISK OF CATCHING CORONAVIRUS
According to the CDC, the immediate risk of exposure to the Coronavirus is low for most people. Additionally, it has been reported that most cases are mild. Those who are at a greater risk for experiencing a severe Coronavirus illness are older people and those with preexisting health conditions such as heart disease, lung disease, and diabetes. If you fall into one or more of those categories, take extra precaution in your Coronavirus prevention.
Remember, just because you may fall into the high-risk category does NOT mean you will catch it. And if you do, it does NOT mean that you will die. It’s important to keep a rational mind about the statistics.
USE CORRECT PREVENTATIVE METHODS
While you can’t control the spread of Coronavirus, you can control how you respond to this situation. The CDC recommends these everyday actions to prevent the spread of illness:
- Avoid close contact with people who are ill.
- Clean frequently touched objects and surfaces.
- Wash your hands often with soap and water. Hand sanitizer is good enough in a pinch.
- Avoid touching your face, especially your mouth, eyes, and nose.
- There’s no need to wear a mask. Save them for medical professionals and those who are ill.
This is a big life lesson of learn to control what we can, and accept what we cannot. Germs spread. It’s actually incredible if you think about it, how much our bodies can take on a daily basis with the germs we come into contact with every day. Our bodies are resilient and self-repair constantly. We know what we need to do to do our best in controlling the spread of all germs.
CREATE A PLAN OF ACTION
Talk with those in your household about what to do if Coronavirus spreads to your community. Assess the needs of each person, especially those who are at an increased risk of developing severe complications. Learn about the resources that are available to you in case you need health care services, information, or any additional support. Stay in contact with your work, your child’s school, and local agencies about any upcoming closings or modifications in gatherings.
If it helps, stock up on some necessary supplies like toilet paper, medications, canned and boxed foods, frozen foods, and other supplies that you may need if in your home for 2-4 weeks. Prior Planning Prevents Poor Performance. This is true in times of uncertainty and can really slow the rise of anxiety.
RECOGNIZE THAT IT’S NORMAL TO BE WORRIED ABOUT THE CORONAVIRUS
Since we do not yet know everything about the Coronavirus, it’s definitely ok to be worried. Having some anxiety might even encourage you to take preventative measures (like washing your hands more than usual) which, in turn, will reduce your risk of getting sick. However, stressing over the fact that you’re anxious about the Coronavirus will only make the cycle worse.
Stress increases cortisol and other hormones that make us eat worse and sleep less. This can lead to being physically and emotionally run down, with or without the Cornoavirus.
These are always good tips in times of stress:
- Get enough rest. Without enough sleep, our brain/body won’t function optimally.
- Maintain a healthy diet. Try to avoid the extra sugar and carbs and stock up on veges and whole foods.
- Get outside. We need some fresh air and nature to help ease anxiety.
- Move your body. Even just running up and down the stairs, going for a walk around the block or doing a dance party with your kids at home can improve mood.
- Yoga or Meditation can calm a busy mind. Start doing this with your children or partner/spouse, have fun with relaxation. Make it part of your day.
- Stay connected. Even in social distancing times, we need to remain connected (at least emotionally) to those we love.
- Power in the Pause. Start to listen to your body. Most of the time, our body knows what we are feeling before “we” know! Stop, breath, listen and be gentle with yourself.
TALK TO A MENTAL HEALTH PROVIDER…VIRTUALLY!
If your anxiety about Coronavirus is surpassing what you can handle, a little therapy won’t hurt. Anxiety often arises during times of uncertainty, but that’s when it’s most important to keep mentally healthy. Therapy can help you manage anxiety about many different things.
In today’s world, tele-mental health (otherwise known as online therapy or eTherapy) allows people to access mental health therapy from the germ-free comfort of their own home or surroundings!
Having excessive anxiety about the Coronavirus will lead to more harm than good. Use preventative methods, make a plan, and know that you’re going to be okay. Always remember that help is available if you need it, for both your physical and mental needs.
Legislative Update: Governor Walz Signs Three Much Needed Executive Orders
Governor Walz Signs Three Much Needed Executive Orders
On Friday afternoon, Governor Walz signed executive orders 20-10, 20-11, and 20-12. These executive actions were absolutely necessary to ensure that mental health programs have the flexibility needed to continue providing services but in alternative ways during the COVID-19 pandemic. A recent article in the Star Tribune, as well as an opinion piece make the need for this action clear.
The most important executive order for the mental health community is EO 20-12. This executive order reflects SF 4200, which is bipartisan legislation that would easily pass on a floor vote if the legislature were able to convene. However, given the uncertainty in the legislature – including a staff person being diagnosed with COVID-19 in the House – Governor Walz correctly recognized the urgency of the situation and took executive action.
EP 20-12 provides the Department of Human Services with short-term flexibility to alter background study requirements, licensing and certification standards, requirements for in-person assessments, eligibility renewal standards for public programs, work or community engagement requirements, service delivery standards including treatment setting and staffing ratios, payment procedures, and more. The most important change for the mental health community relates to telehealth, where the executive order allows for flexibility regarding telehealth and other electronic strategies for communicating with providers or patients. Private plans in Minnesota have already agreed to reimburse telehealth from a person’s home and by phone.
This means that a community-based mental health provider will be able to bill for services provided via telehealth, even if this is a phone call and not the more intensive telehealth systems that would usually have to be used. This will increase much-needed mental health access while ensuring that healthcare providers and people with mental illnesses can follow best practices to avoid contracting COVID-19. Many people with mental illnesses don’t have computers or smartphones and people in rural Minnesota don’t have Internet. This step, allowing services by phone, was a top priority for NAMI Minnesota.
More detailed information on how DHS will be implementing the orders will be placed on the DHS website in the coming days.
EO 20-11 was also issued on Friday and allows the Department of Human Services to seek federal authority to waive or change federal requirements for all programs and services, including the Minnesota Family Investment Program (MFIP), Medical Assistance, MinnesotaCare, and other programs to maximize federal funding, maintain enrollee coverage and provider participation, and to ensure public health and safety.
The other order issued on Friday was EO 20-10, which prohibits price gouging for essential goods and services including food, gasoline, medical supplies, health care goods like hand sanitizer, and other essentials.
It’s important to know that your emails made a difference! Special thanks to senate leaders – Abeler, Hayden, and Marty and house leaders – Schultz, Liebling, Kiel, Albright, and Schomacker. We now have bipartisan support for this action in both the House and Senate.
More needs to be done at Federal Level on COVID-19 Response
As the Senate prepares the third in a series of COVID-19-related relief bills, please urge Senator Klobuchar and Senator Smith to ensure people affected by mental illness can maintain their treatment, get health and mental health coverage, access needed support, and lift up the nonprofits they depend on, like NAMI.
We need you to ask your U.S. Senators to do 4 things:
1. Remove barriers to mental health treatment. People need ways to manage existing mental health conditions and maintain mental wellness while reducing their exposure to the coronavirus. To do this, Congress should:
- Eliminate all barriers to widely implementing telehealth in all public and private health plans and encourage all health plans to provide extended supplies and/or mail order refills of prescriptions. Both actions will help people with mental illness avoid the risk of exposure to COVID-19.
- Approve funding for Emergency Response Grants at the Substance Abuse and Mental Health Services Administration (SAMHSA) to assist states in continuing to provide treatment for people with mental health conditions and substance use disorders.
2. Promote coverage for health and mental health care. People with mental health conditions are often uninsured or face barriers to getting needed treatment and support. These challenges are even greater during a crisis. To address this, Congress should:
- Immediately launch a special enrollment period for commercial health insurance in the Marketplace (HealthCare.gov) to make sure people have access to affordable, quality healthcare coverage.
- Require the use of “presumptive eligibility,” which allows certain providers like hospitals and clinics to enroll people in Medicaid that they believe meet eligibility criteria.
- Ensure free COVID-19 testing and treatment for everyone, including people who are uninsured.
3. Ensure safe housing for people with severe mental illness. Many people with severe mental illness experience homelessness or housing insecurity and are uniquely vulnerable to being exposed to the virus and outbreaks in shelters or encampments. With the loss of steady income, many more individuals are also at risk of losing housing. Congress must act by:
- Providing $5 billion to serve people who are homeless and help them stay safe and healthy during this emergency.
- Approving an additional $5 billion to provide rapid rehousing for people who are at immediate risk of becoming homeless and funding for rental assistance to help low-income renters weather this crisis.
- Putting a temporary stop on evictions to ensure that renters and homeowners maintain stable housing during this crisis.
4. Support nonprofits’ capacity to serve. The economic impact of this crisis will also touch charitable organizations like NAMI organizations and our partners. Nonprofits need support to meet greater demand and fill important gaps during this time. To assist, Congress should:
- Provide targeted assistance to 501(c)3 organizations to help them keep their doors open during this crisis and offer paid leave to their employees.
Senator Klobuchar and Senator Smith need to hear from you TODAY. Please contact them now to ensure people with mental illness are helped in their response to COVID-19.
News from the State Level
COVID-19 Update
NAMI Minnesota is working very hard to ensure that our members and supporters have access to the most up-to-date information about COVID-19 and the resources that are available. All this information is available at NAMI Minnesota’s website. Please also note that our support groups have been moved online and many classes are being scheduled online as well.
Special Open Enrollment Period for MNsure
In response to the COVID-19 pandemic, MNsure has opened a special enrollment period to obtain health insurance on the private marketplace. Starting on March 23rd, any Minnesotan can apply for health insurance on MNsure for coverage starting on April 1, with a deadline of April 21st to get coverage under this special enrollment period. Here is the broad eligibility criteria:
- This special enrollment period is for eligible Minnesotans who do not have current health insurance.
- You do not need to be sick to qualify.
- If you are currently enrolled in a plan through MNsure, you cannot use this special enrollment period to change plans.
To learn more about this opportunity, all you have to do is go to MNsure’s website.
Governor Walz Signs Executive Order on Elective Surgeries
Governor Walz signed another executive order in response to the COVID-19 pandemic, requiring health-care providers to postpone elective surgeries, including elective dental procedures. This will reduce the strain on Minnesota’s health care system will experience and is in alignment with recommendations from the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services (CMS). The executive order defines a non-essential or elective surgery as a procedure that can be delayed without undue risk of the current or future health of the patient. Potential criteria to consider when determining if a procedure is elective can include:
- Threat to the patient’s life if the surgery or procedure is not performed
- The threat of permanent dysfunction of an extremity or organ system, including teeth or jaws
- Risk of metastasis or progression of staging
You can read the full executive order here.
News from Federal Level
Federal Action on COVID-19 Outbreak
This week, Congress and President Trump were able to reach a compromise and pass H.R. 6201. While we can expect the passage of additional legislation in the near-term, this marks the first spending bill made in response to the COVID-19 pandemic. This legislation includes a number of funding increases and short-term policy waivers that will help people access the supports they need during the pandemic. Here are the key changes that NAMI members should be aware of:
Food and Nutrition:
- $500 million to provide nutritious food to low-income pregnant women or mothers with young children who lose their jobs due to COVID-19
- $400 million to meet the increased demand at local food banks, with $100 million set aside to support the storage and transportation of food.
- Allows the Department of Agriculture to approve state plans to provide emergency food stamps to children who qualify for free or reduced lunch when the child’s school has been closed for at least 5 consecutive days.
- $100 million for food assistance to U.S. territories.
- $250 million for a senior nutrition program to provide 25 million additional home-delivered and pre-packaged meals to low-income seniors who are homebound, have disabilities, have multiple chronic illnesses, or are caregivers for seniors who are homebound.
- Work and work training requirements are suspended for low-income jobless workers on food stamps.
- Allows states to request a waiver in order to have additional flexibility with food stamp benefits.
Emergency Paid leave
- In order to be eligible, the person must have been employed for 30 or more days before they were impacted by COVID-19, work for an employer with fewer than 500 employees, and meet one of these criteria
- Worker has a COVID-19 Diagnosis
- Worker is quarantined on the recommendation of health care provider, employer, or government official to prevent the spread of COVID-19
- Worker is caring for someone with COVID-19 or under quarantine
- Worker is caring for a child or another individual who is unable to care for themselves due to the COVID-19 related closure of a school, child-care facility, or other care programs.
- This benefit will be available for up to three months when the employee had to take more than 14 days of leave from their work in response to COVID-19.
- The benefit will amount to two-thirds of an individual’s average monthly earnings up to $4,000 and must be offset by any state or private paid-leave benefit the individual receives.
- SSI benefits do not count as income or resources for the purposes of this program.
Unemployment Benefits
- $1 billion for emergency grants to the states related to processing and paying unemployment insurance benefits.
- For states that experience an increase of 10% or more in its unemployment rate, the federal government will pay for 100% of the costs for extended benefits, which normally requires 50% funding from the states.
Paid Sick Leave
- All employers with fewer than 500 employees must allow workers to gradually accrue seven days of paid sick leave, as well as offer 14 days of sick leave immediately following a public health emergency.
- Paid sick days cover staying home when a child’s school is closed due to a public health emergency, when the employer is closed due to a public health emergency, or if you or a family member is quarantined or isolated due to a public health emergency.
- The federal government will reimburse small businesses with 50 or fewer employees for the costs of providing the additional 14 days of sick leave.
Health Insurance
- Requires private health plans and Public Health Plans to cover COVID-19 testing without any cost-sharing by the enrollee.
- The federal government will pick up costs related to COVID-19 testing for people without health insurance.
National Council Breakdown of CMS Actions on COVID-19
CONDUCTING TELEMEDICINE VISITS
CMS has clarified and provided more flexibility for states to respond to the coronavirus. The allowances outlined below will remain effective for the duration of the COVID-19 public health emergency.
Medicaid Telehealth
- CMS made clear to states that they already have the flexibility to utilize telehealth services, including audio-only services, in their Medicaid programs. States can cover telehealth using various methods of communication such as telephonic, and video technology commonly available on smartphones and other devices. No federal approval is needed for state Medicaid programs to reimburse providers for telehealth services in the same manner or at the same rate that states pay for face-to-face services.
- Note: States themselves, not CMS, are responsible for making these options, including audio-only telephonic services, available to providers.
Telehealth and Prescriptions of Controlled Substances: The DEA has announced that for the duration of the public health emergency, registered practitioners may issue prescriptions for controlled substances to patients for whom they have not conducted an in-person medical evaluation, providing the following conditions are met:
- The prescription is issued for a legitimate medical purpose by a practitioner acting in the usual course of his/her professional practice
- Telemedicine communication is conducted using an audio-visual, real-time, two-way interactive communication system.
- The practitioner is acting in accordance with applicable Federal and State law.
This temporary relief of the Ryan Haight Act has been a long-term advocacy goal of the National Council and its members. We thank all members who worked to build this case with DEA over the years to make this emergency declaration possible.
Medicare Telehealth
- Retroactive to March 6, Medicare will temporarily pay clinicians to provide telehealth services for beneficiaries across the country. Previously, Medicare only covered particular services in specific situations, such as if an enrollee lived in a rural area and was unable to receive in-person services within a reasonable distance. A range of providers, including clinical psychologists and licensed clinical social workers, will be able to offer Medicare-covered telehealth services to enrollees based in any health care facility, including physicians’ offices, nursing homes, as well as from enrollees’ homes.
- Additionally, the Families First Act corrects language included in Congress’s first COVID-19 response package to clarify that, for the purposes of establishing a relationship with a provider to waive current prohibitions surrounding telehealth services in Medicare, any services allowable under Medicare will qualify as an existing relationship, even if Medicare was not the program paying for the service.
Telehealth Best Practices
The National Council has compiled a reference document that includes details on these changes and more, titled “Best Practices for Telehealth During COVID-19 Public Health Emergency.” This document is intended to provide mental health and substance use treatment providers with the background and resources necessary to help begin or expand the use of telehealth.
TELEHEALTH AND PRIVACY: HIPAA & 42 CFR PART 2
HIPAA: The Office for Civil Rights (OCR) at the Department of Health and Human Services (HHS) announced that it will exercise its enforcement discretion and will waive potential penalties for HIPAA violations against health care providers that serve patients through everyday communications technologies during the COVID-19 public health emergency. This applies to widely available communication apps such as FaceTime or Skype when used in good faith for any telehealth treatment or diagnostic purpose, regardless of whether the telehealth service is directly related to COVID-19.
42 CFR Part 2: SAMHSA issued guidance related to the sharing of substance use disorder health records throughout the public health emergency. SAMHSA makes clear in the guidance, information disclosed to the medical personnel who are treating such a medical emergency may be re-disclosed by such personnel for treatment purposes as needed. SAMHSA notes that Part 2 requires programs to document certain information in their records after a disclosure is made pursuant to the medical emergency exception. SAMHSA emphasizes that, under the medical emergency exception, providers make their own determinations whether a bona fide medical emergency exists for purpose of providing needed treatment to patients.
INCREASED HEALTH FUNDING
- Federal Medicaid Funds: The federal government’s share of Medicaid payments, known as the Federal Medical Assistance Percentage (FMAP), has been increased by 6.2 percentage points. This increased assistance comes with the requirement that state Medicaid programs cover COVID-19-related treatment, vaccines, and therapeutics at no cost to enrollees as well as states not making eligibility standards more restrictive or increasing any cost sharing for enrollees.
- More Funding for CDC & NIH: The Trump Administration is updating its Fiscal Year 2021 Budget Request to include a request for an additional $45.8 billion and the necessary authorities for the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH) to address ongoing preparedness and response efforts.

